Welcome to the general otology section of our website. While many patients come to UCSF because they have rare and complicated diseases, we also care for some of the more common ear problems, like hearing loss, tinnitus, or ear infections. This section of our website contains informational content for patients about some of these common problems. Of course, information on a website can never substitute for a medical opinion from a qualified professional, but we do hope that you will find this information interesting and helpful.
Specific Otologic Diseases
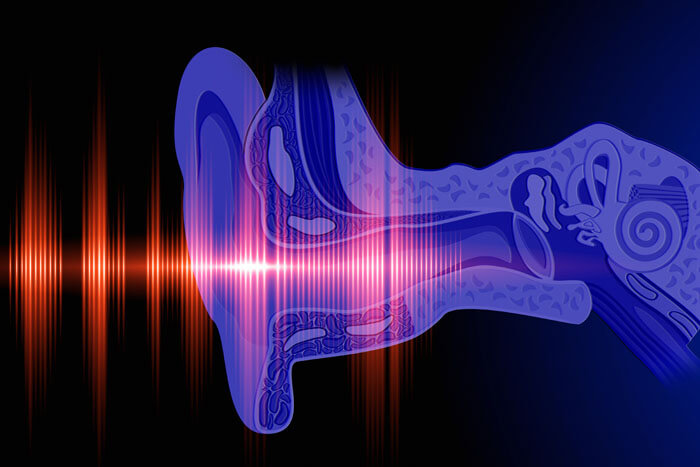
Normal hearing depends on an efficient transfer of sound wave energy from the air, to the eardrum, through the hearing bones, and into the cochlea. If there is any problem along that pathway, then a hearing loss can result. So, a conductive hearing loss can occur at any point along the sound conduction pathway, including the ear canal, ear drum (tympanic membrane), and ear bones (ossicles). We use the term “conductive”, because the problem stems from impaired sound conduction. In general, there are usually several options for treatment of “conductive” hearing loss. Firstly, the underlying cause for the hearing loss can be fixed. For example, if there is a hearing loss due to fluid filling the middle ear, then a PE (pressure equalization) tube can be placed into the eardrum, to allow the ear to fill back up with air, which is its normal state. In children, this is done in the operating room, but in adults ear tubes can be placed in the clinic, with minimal discomfort. Secondly, a hearing aid can be used. It’s important to know that some causes of conductive hearing loss, like a cholesteatoma, can be dangerous, and therefore a patient should obtain medical clearance before using a hearing aid for a conductive hearing loss. Thirdly, observation is also a treatment option in many cases, provided that a qualified practitioner has determined that the cause of the hearing loss is not dangerous to the patient.
Normally, sound waves vibrate the three ear bones (ossicles) in succession: the malleus, the incus, and the stapes. The stapes sits between the incus bone and the inner ear, held in place by a ligament that encircles the base of the stapes bone. This allows the bone to vibrate efficiently, thereby conducting the sound vibrations to the organ of hearing (the cochlea). In otosclerosis, abnormal bone overgrows the base of the stapes bone, cementing it in place. This prevents the stapes from vibrating normally, and results in a conductive hearing loss. In a small percentage of cases, there is an exuberance of abnormal bone overgrowth, around the stapes and the inner ear, and this can also cause a mixed hearing loss (partially conductive, partially sensorineural). Some patients will have an affected family member as well. The diagnosis is made based on a hearing test (audiogram), examination of the ear, and tuning fork test. There are three reasonable treatment options: observation, hearing aids, or surgery. Surgery is typically performed through the ear canal, without visible incisions, and is outpatient (go home the same day). While there are always risks to any surgical procedure, surgery for otosclerosis is considered highly safe and highly effective. It involves removing the diseased parts of the stapes bone, and replacing it with a prosthesis.
Otitis Externa: In otitis externa, the external ear canal become infected. This is also called swimmer’s ear, because water exposure is a common cause for the infection. Other causes that allow bacteria to penetrate the ear canal skin include local trauma, and skin conditions like eczema. The infection of the ear canal can cause swelling of the ear canal skin, pain, hearing loss, and drainage. Since the ear canal is one of the most sensitive areas of the body, the pain associated with otitis externa can be quite severe. Treatment is with antibiotic ear drops, which are highly effective. Occasionally, if the ear canal is swollen shut, such that drops can’t get in, a wick will be placed. This is a micro-sponge that allows the ear drops to soak the infected skin, and to get into the deeper parts of the ear canal.
Otitis Media: refers to infection or inflammation of the middle ear space. The middle ear is the area behind the eardrum, where the ear bones are located. During otitis media, the middle ear can fill up with fluid, pus, or inflammation tissue. Symptoms including pain, hearing loss, and ear pressure. For acute otitis media, which refers to a sudden infection of the ear with pus, treatment is with oral antibiotics. For otitis media with effusion, in which the middle ear is filled with fluid, ear tubes are often placed if the fluid does not resolve by three months.
Chronic Suppurative Otitis Media (CSOM): In this condition, the ear is chronically infected. That means that an infection persists for longer than three months. There is a perforation in the eardrum, and frequent drainage. The drainage can be bloody, purulent, and foul smelling. Sometimes this is seen by itself, and sometimes its seen in association with a cholesteatoma (see the cholesteatoma section). Treatment begins with medical therapies to treat the infection, including topical antibiotics (ear drops). However, in many cases, surgery is required to clear out sequestered pockets of infection, inflammation, and scar tissue, and to restore the ear to health.
Malignant Otitis Externa (MOE): also referred to as osteomyelitis of the skull base, is a serious infection of the ear canal and the surrounding tissues. Unlike with otitis externa, in malignant otitis externa the infection has spread beyond the skin of the ear canal, to involve the bone of the skull, and the surrounding soft tissue and cranial nerves. Therefore, patients can have ear pain, drainage, and hearing loss, just like regular otitis externa, but also other signs that indicate a deeper infection, such as facial palsy, dizziness, double vision, and fevers. An accurate diagnosis is essential, because treatment requires not just topical antibiotics (ear drops), but also oral or intravenous antibiotics. Laboratory testing and imaging are generally required to assess the extent of the infection. Most commonly, patients have a condition that predisposes them to bad infections, such as diabetes. Many patients are initially treated in the hospital, before transitioning to at home care with close follow up.
The Eustachian tube connects the middle ear cavity and the nasopharynx (the far back of the nose). It is the primary way that are ears are able to equalize. This normally occurs when we swallow, because of a pulley like system that pulls the Eustachian open when the palate moves during the swallow. Therefore, the Eustachian tube is normally closed, but to have a healthy ear, it needs to frequently open during the day. This creates two categories of Eustachian tube dysfunction: firstly, and far more commonly, when the Eustachian tube does not open properly, and is therefore too closed, and secondly, and far less commonly, when the Eustachian tube does not close properly, and is therefore too open.
First, let’s discuss the common problem where the Eustachian tube does not open well, and therefore the ear is unable to equalize. This can cause a host of problems, including chronic middle ear pressure, ear fluid, eardrum perforations, eardrum collapse (atelectasis), infections, and cholesteatoma (see below). The medical assessment involves looking for any contributing factors that could be causing Eustachian tube blockage, such as sinusitis, allergies, or growths in the nasopharynx, and these should be treated if present. In addition, treatment involves regiments to help the ear equalize (like frequent Valsalva maneuvers where the ear is “popped”), or ear tubes. Ear tubes usually work well for Eustachian tube obstruction, because the middle ear is given an alternate and more direct way to equalize. A newer treatment for Eustachian tube obstruction is balloon dilation of the Eustachian tube. During this procedure, which is done under anesthesia, an inflatable balloon is introduced into the Eustachian tube, and inflated. This causes the Eustachian tube to scar into a more open position, thereby restoring its function. While this is still a new treatment, our early experience has shown that’s relatively safe and effective.
In patulous Eustachian tube, which is quite uncommon, the opposite problem occurs and the Eustachian tube is too open. Normally, because the Eustachian tube is closed, we are acoustically shielded from many of our own internal sounds, like breathing, or hearing our voice. When the Eustachian tube is open all the time, this changes how we hear these internal sounds, which become a lot more noticeable. Many patients describe this new and distressing hearing situation similar to hearing sounds in a tightly enclosed space, like a barrel. Needless to say, this can be quite awful. Treatment involves medical and surgical treatments to restore the Eustachian tube to its normal state of being closed most of the time, except for when we periodically equalize when we swallow.
A cholesteatoma is a cyst composed of skin debris in the middle ear space. There are many theories for why they occur, which seems to be most commonly because parts of the eardrum near the hearing bones collapse inward, and then the skin lining of the eardrum and ear canal get turned inward into a cavity, which expands as the skin keeps shedding. It’s important to know that a cholesteatoma is not a cancer, but instead a skin cyst in the ear. They do behave like benign tumors, eroding through nearby structures, like the bone of the ear canal, the hearing bones, the facial nerve, the organs of hearing and balance, and the brain. Therefore, cholesteatoma can cause hearing loss, ear infections, ear drainage, facial palsy, dizziness, pain, brain infections, and spinal fluid leakage. They do grow slowly, over months to years. Given this possibility of serious consequences from the cholesteatoma, treatment is almost always advised, which involves surgery to eradicate the cholesteatoma, and rebuild the hearing mechanism.
We all produce earwax, just like we all have mucous in our noses. The function of ear wax is to keep the ear canal clean, by trapping debris, which slowly migrates outward. Therefore, it’s important to know that almost all normal humans: will continuously make earwax their whole lives, and that earwax will continuously come out their ear canals. Therefore, almost all people don’t need to worry about their ear wax, and don’t need to treat it. In a few patients, earwax buildup is so bad that it causes hearing loss. This is called a cerumen impaction. In cases like that, the earwax should be removed, either with drops, or with a qualified medical professional.
We are frequently asked a few questions about earwax:
- Are Q-tips bad for me? In most cases, Q-tips are harmless, although they do tend to push earwax deep into the ear canal, onto the eardrum, in addition to ear wax that is removed. However, every ear doctor has seen cases where Q-tips really harmed someone’s ear. This can be laceration to the ear canal, a perforated eardrum, or even deeper damage, with permanent hearing loss and dizziness. Therefore, in general, we think it best to have you avoid putting anything into your ear canals.
- What should I do to prevent earwax? Earwax cannot be prevented, it’s a normal part of being human!
- What should I do to treat earwax? In most cases, unless you have severe earwax that causes a hearing loss, earwax can be left alone, and the earwax that comes out of the ear canal can be cleaned in the shower.
Once sound waves pass through the ear canal, the eardrum, and the hearing bones, then enter the organ of hearing, which is the cochlea. In the cochlea, sound waves are transformed by hair cells into electric signals that are conducted along the hearing nerve into the brain. Therefore, the cochlea is considered the “sensory” organ of hearing. Patients who have hearing loss due to problems with either the cochlea, or the hearing nerve, are said to have “sensorineural” hearing loss. This is in distinction to conductive hearing loss, which is discussed above. Sensorineural hearing loss is incredibly common, especially as we get older. Common causes include: aging, noise exposure, and genetic causes (especially in children). Uncommon causes include a disease where hearing is suddenly lost in one ear (sudden sensorineural hearing loss), Meniere’s disease, tumors like vestibular schwannoma (this is a concern with unilateral, or one sided hearing loss), medications that can damage the inner ear, trauma, neurologic disease, and autoimmune diseases. Sensorineural hearing loss can be treated with hearing aids, or in more severe cases with cochlear implants. More information on cochlear implants can be found here.
This is a hole in the eardrum. Since the eardrum is used to help collect and concentrate sound waves, a hole in the eardrum usually causes hearing loss. In addition, patients can get ear infections, because the eardrum normally protects the middle ear from bacteria. In most cases, the perforation is not dangerous, and treatment options include observation, surgical repair, or hearing aids. However, in some cases, the perforation can be a source of infections, or can all for the growth of cholesteatoma. In those cases, surgical repair is advised. Surgical repair, called “tympanoplasty”, involves using a graft to repair the eardrum. The success rate is high, around 90%. Usually the surgery is done as an outpatient, meaning you go home the same day. Depending on surgeon preference and the configuration of the perforation, surgery can either be done though the ear canal, or it may require an incision behind the ear.
Tinnitus is covered more in detail here. It is broadly defined as hearing a sound, in the absence of external sounds. It’s important to distinguish “pulsatile tinnitus”, in which the sound heard is the pulse or heartbeat, which sounds like a “whooshing” that coincides in timing with one’s own pulse. There is usually a cause found for pulsatile tinnitus, and since some of the causes can be dangerous, medical consultation and workup are almost always advised. With most cases of tinnitus, the sound that is heard does not pulse, although it can certainly fluctuate. There are a variety of sounds that can be heard, including ringing, hissing, static, buzzing, etc. Tinnitus appears to be the brain’s response to hearing loss. Because the sound represents the brain’s response to altered sensory input, the usual treatments involve restoring
hearing (like with a hearing aid), counselling, and masking the tinnitus sound with other sounds. It’s important to know that at this point in time, there is no cure for tinnitus, but there are quite a few treatment options which can be effective.
Tumors in the ear are relatively uncommon. The most common type of ear tumor is a glomus tumor, which is a vascular tumor that arises from neuroendocrine cells. The first symptom is usually hearing your pulse, because the tumor has such a good blood supply that it actually pulses. With a glomus tympanicum, the tumor is usually confined to the middle ear space. With glomus jugulare tumors, there can be tumor involvement of the middle ear, mastoid, skull base, neck, and brain cavity. The cranial nerves, which are important for speech, swallowing, and facial movement, can be involved with tumor.
Small tumors are usually treated with surgery. With larger tumors, we take an individualized approach, taking into account a patient’s age, medical status, tumor size, cranial nerve status, and patient wishes. Together, we are able to formulate a treatment plan, which can involve surgery, radiation therapy, or observation.
